Imagine simulating a patient’s entire physiological system or predicting hospital resource demands weeks in advance – all before anything happens in the real world. That’s the power of digital twins in healthcare.
Borrowed from manufacturing and aerospace, the digital twin concept is now reshaping how we think about patient care, hospital operations, and clinical research. By creating real-time, data-driven virtual replicas of people, devices, or systems, healthcare providers can move from reactive to predictive and even preventive approaches.
As data becomes more abundant – from wearables, EHRs, imaging, and IoT devices – the opportunity to apply digital twins across healthcare is not just exciting – it’s becoming essential. In this article, we’ll walk through the most transformative and practical use cases of digital twins in healthcare, highlighting how they’re solving long-standing challenges and opening new doors in personalized care, resource optimization, and innovation.
Why Healthcare Needs Digital Twins?
Healthcare is facing a perfect storm of rising patient loads, chronic disease prevalence, clinician burnout, and mounting operational inefficiencies. Traditional models of care delivery – largely reactive and fragmented – are struggling to keep pace with this complexity.
Enter digital twins: virtual replicas of physical entities, fueled by real-time data and advanced simulations. In healthcare, these twins can mirror anything from a single patient’s heart to an entire hospital system. They integrate data from medical records, imaging, wearables, genomics, and IoT devices to simulate behavior, test scenarios, and predict outcomes.
The need is clear: better decision-making, early intervention, and precision treatment aren’t just aspirations – they’re now possible. The benefits of digital twins for patient care help bridge the gap between data and action. They help clinicians personalize care, optimize surgical planning, and pre-empt system bottlenecks. For health systems looking to reduce costs without compromising outcomes, this technology offers a proactive lens on both care and operations.
What follows are 10 real-world use cases where digital twins are not just theoretical – they’re transforming how healthcare is delivered, managed, and improved.
10 Powerful Use Cases of Digital Twins in Healthcare
Digital twins are no longer futuristic concepts in medicine – they’re actively transforming how care is delivered, optimized, and scaled. By creating real-time digital replicas of physical entities like patients, organs, hospital systems, and medical devices, healthcare providers are stepping into an era of proactive, personalized, and predictive care. Below are ten high-impact ways digital twins are being used across healthcare, with immersive explanations to help you envision their real-world impact.

1. Precision Treatment Planning for Chronic and Complex Diseases
Chronic illnesses like cancer, diabetes, and autoimmune disorders often follow unpredictable trajectories. Traditional treatment models, based on static test results and population averages, fall short in anticipating how an individual patient may respond. Digital twins change that.
By integrating longitudinal data – clinical records, lab tests, wearable data, genomics, and imaging – doctors can create a living, breathing digital replica of a patient. On this twin, they can simulate different treatment options and predict responses in real time. In a recent hospital trial, oncologists used digital twins to test various chemotherapy combinations on a breast cancer patient’s profile. They selected a regimen that minimized toxicity while maximizing tumor suppression – significantly improving the patient’s quality of life.
2. Surgical Planning and Risk Simulation
Every surgery carries risk – but what if surgeons could rehearse the procedure multiple times in a hyper-accurate simulation before entering the OR?
That’s exactly what answers how digital twins are used in healthcare. When a patient is scheduled for complex surgery – such as brain tumor removal or congenital heart repair – surgeons can generate 3D anatomical models from MRI and CT data and simulate every incision, movement, and tool interaction on the twin. In one renowned hospital, neurosurgeons virtually tested several routes to remove a deep-seated tumor. The selected approach avoided key nerves and blood vessels, reducing both operating time and post-op complications. The patient recovered 40% faster than the department’s average for similar cases.
3. Proactive Management of Chronic Conditions
In diseases like heart failure or COPD, early intervention often prevents emergencies. But how can care teams detect subtle declines before symptoms show?
With digital twin applications constantly synced to wearable devices, clinicians can monitor a patient’s twin in near real time. Changes in breathing rate, blood oxygen, or heart rhythms – however minor – are reflected instantly. One health system piloting this approach found that in 82% of cases, the twin flagged deterioration days before patients noticed. Early medication adjustments and remote check-ins drastically reduced hospital readmissions and emergency visits.
4. Accelerated Drug Discovery and Testing
Bringing a new drug to market takes over 10 years and costs billions, largely due to slow and risky clinical trials. Digital twins help pharma teams fast-track this process without compromising safety.
By simulating thousands of digital patients – each with different genes, lifestyles, and co-morbidities – researchers can test drugs in virtual trials before ever involving humans. In a diabetes research program, digital twins were used to model how a new insulin formulation would work in patients with varying BMI, kidney function, and insulin resistance. This helped the team identify the safest dosage range and eliminate a risky compound, shortening the trial phase by 7 months and saving millions in operational cost.
5. Immersive Training and Real-World Readiness
Medical training is often limited to textbooks, mannequins, or low-fidelity simulations. But real patient care is messy, high-pressure, and unpredictable.
With digital twin applications, hospitals can recreate realistic scenarios based on actual clinical data and patient histories. One training facility created a virtual ICU using past records of emergency cesarean sections complicated by cardiac arrest. Medical interns and nurses practiced dozens of scenarios on the twin model, testing not just medical decisions but team dynamics and timing. After implementation, that hospital recorded a 25% improvement in maternal emergency response time and better overall care coordination.
6. Smarter Hospital Operations and ICU Demand Forecasting
Hospital overcrowding is a recurring crisis – especially in ICUs where capacity planning can make or break patient outcomes. Here, digital twins of hospital infrastructure help administrators simulate future demand based on current trends.
Using a healthcare digital twin model that pulls data from EHRs, weather forecasts, regional disease patterns, and staffing schedules, one hospital predicted a 3-day surge in pneumonia admissions during flu season. It activated additional ICU beds, rescheduled elective procedures, and alerted neighboring facilities. The result: not a single patient had to be turned away or wait for a critical bed.
7. Rehabilitation Tailored to Patient Recovery Pace
Post-surgical or neurological rehab is highly variable. Some patients progress fast; others need more time and support. Digital twins help therapists personalize care based on real recovery data.
A patient recovering from ACL reconstruction wore motion sensors during daily exercises. The healthcare digital twin tracked joint movement, muscle stress, and balance patterns, identifying when she was overcompensating or underperforming. Her therapist modified the plan weekly based on this input, avoiding setbacks and enabling her to return to sports two weeks ahead of schedule.
8. Predictive Maintenance of Critical Medical Equipment
When medical devices fail, lives are at risk. Digital twins of hospital assets – like ventilators, dialysis machines, or infusion pumps – can forecast mechanical wear and tear.
A large hospital chain used twins to track internal pressure levels and temperature fluctuations in its dialysis machines. When the system detected abnormal friction in a batch of machines, it flagged the maintenance team. Preventive service was done before breakdowns occurred – avoiding treatment interruptions and boosting equipment uptime by 18%.
9. Continuous Behavioral Health Monitoring
Mental health symptoms often fluctuate subtly – until a breaking point is reached. There are several healthcare digital twin use cases that allow therapists to spot warning signs early by combining patient journals, sleep tracking, therapy session transcripts, and biometric signals.
For a bipolar patient, the twin noticed reduced social engagement (from phone usage), rising heart rates during sleep, and erratic messaging patterns. These signs preceded a manic episode. The therapist was notified, leading to a timely intervention and medication adjustment that helped stabilize the patient without hospitalization.
10. Crisis-Ready Emergency Response Networks
Ambulance routes, ER workflows, and triage protocols must run like clockwork – but they often don’t. To optimize emergency response across a city, one hospital created a digital twin of its entire response network, pulling in data from traffic feeds, call logs, and hospital occupancy in real time.
During a major city marathon, the twin predicted probable hotspots for incidents and redistributed ambulances accordingly. Despite a 40% spike in calls, average response times dropped by 22%, thanks to proactive route planning and load balancing. Patients reached care faster, and ER teams were better prepped for incoming cases.
How to Start Building Digital Twins in Healthcare?
Launching a digital twin solution in healthcare begins with precision – not code. The first step is to define the exact entity or system you want to replicate: is it a virtual model of a patient’s cardiovascular system, a hospital’s resource allocation framework, or a high-risk medical device? The clearer your objective, the more effectively you can map the necessary data sources, simulation models, and real-time interactions.
Next comes data strategy. Digital twins thrive on quality, not just quantity. You need structured and unstructured data from EHRs, wearables, imaging systems, sensors, and potentially even genomics – all normalized and integrated. Privacy and compliance aren’t optional either. HIPAA, GDPR, and other regional regulations must be baked into the architecture from day one.
Then, it’s about choosing the right modeling approach for the healthcare digital twin use cases. For patient twins, you might need physiological simulation engines. For hospital twins, discrete event simulations or system dynamics may be more appropriate. AI and ML models should be layered only after the foundational simulation logic is in place, not as a shortcut to avoid complexity.
Interoperability is the next challenge. Your digital twin must plug into hospital information systems, device interfaces, and diagnostic tools in real time. APIs, HL7/FHIR protocols, and IoT compatibility are critical considerations.
Finally, test small. Build a minimum viable twin – a lean version that replicates a subset of the system – and run it against historical and live data. This controlled environment will allow you to calibrate the model, measure impact, and scale with confidence.
Digital twin development is as much about strategic clarity and domain expertise as it is about engineering. And in healthcare, getting that balance right isn’t optional – it’s lifesaving.
Challenges to Look Out For
Building digital twin technology in medicine is not just a tech initiative – it’s a high-stakes balancing act across regulation, data, and clinical precision. Here are some of the key hurdles developers and healthcare providers should be prepared for:
- Data fragmentation and quality issues
Healthcare data is notoriously siloed. Pulling together EMRs, imaging files, IoT signals, and lab reports into a single, usable stream is no small feat. Often, the data is inconsistent, incomplete, or collected in incompatible formats – making it difficult to build accurate and reliable digital replicas. - Privacy, compliance, and ethical risks
Healthcare digital twins require sensitive patient data, which brings with it complex regulatory obligations. Maintaining compliance with HIPAA, GDPR, and local data protection laws – while still enabling real-time data sharing and analytics – is a significant challenge. Plus, the ethics of simulating patient scenarios or predicting health outcomes can trigger sensitive debates around data use and medical consent. - Real-time integration complexity
Digital twins need to reflect real-world changes as they happen. But hospitals and healthcare systems often lack the IT infrastructure for seamless, real-time data flow. Integrating multiple legacy systems with modern APIs or IoT sensors demands both technical depth and operational agility. - Lack of cross-functional expertise
Digital twins don’t just require developers – they need a mix of clinical experts, data scientists, systems engineers, and UX designers working in close alignment. Finding or assembling such multi-disciplinary teams is both costly and time-consuming, and misalignment can stall progress entirely. - High development and maintenance costs
Sophisticated simulations, real-time analytics engines, and secure cloud infrastructure don’t come cheap. Add ongoing model updates, validation cycles, and maintenance, and the cost can quickly spiral. Without a clear ROI or reimbursement pathway, many organizations hesitate to move beyond pilots. - Resistance to adoption in clinical settings
Healthcare professionals are already overwhelmed with tools and systems. Convincing them to trust – and use – a digital twin interface often requires evidence, training, and time. Without early stakeholder buy-in, the most technically sound twin may go unused.
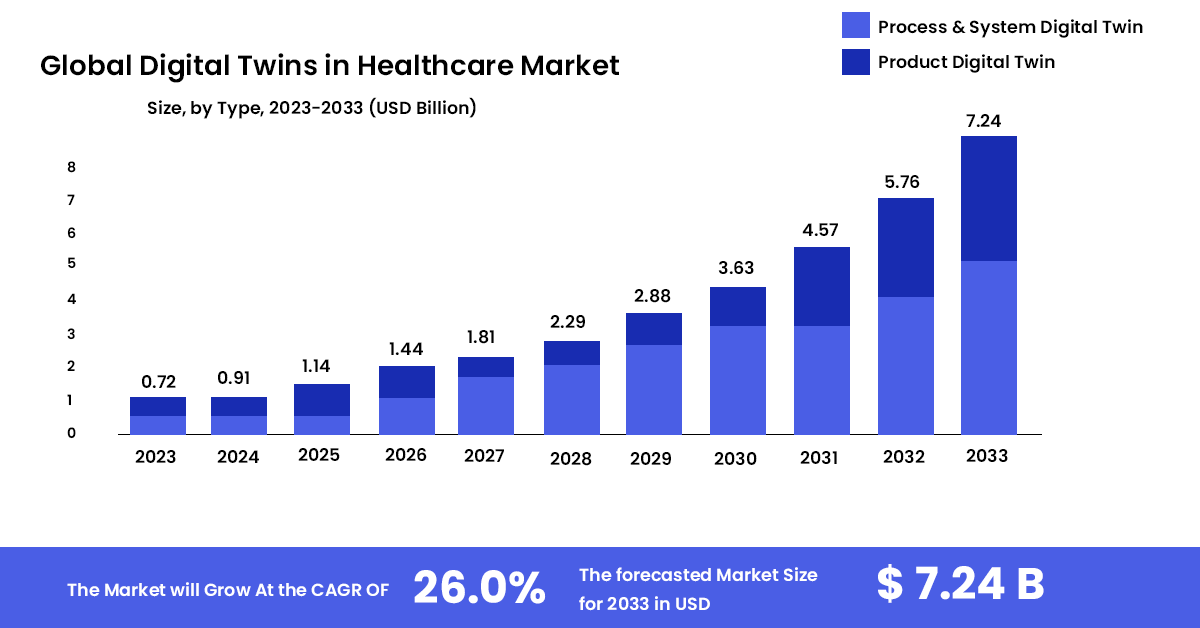
The Future of Digital Twins in Healthcare
Digital twins are on the verge of redefining how healthcare systems predict, personalize, and deliver care. As their foundation matures – richer data pipelines, more accurate simulations, better AI interpretability – they are poised to evolve from isolated pilots into core infrastructure across hospitals, research institutions, and even patient homes.
One of the most promising shifts will be the transition from reactive to preventive healthcare. With highly individualized patient twins, care teams can foresee complications before they emerge, test interventions in a simulated environment, and fine-tune treatment plans accordingly. For chronic diseases, this could mean continuous, adaptive management tailored to daily biometric inputs rather than quarterly clinic visits.
Beyond patient care, digital twins will also become critical in clinical trial acceleration. Pharma companies can test drug interactions, dosage variations, or population responses on virtual cohorts long before human trials begin. This could significantly reduce costs, compress timelines, and improve trial safety.
In hospital operations, next-gen twins will optimize everything from emergency room workflows to bed availability. By running predictive models on thousands of operational scenarios, hospitals will be better equipped to handle patient surges, resource constraints, or system failures – even before they occur.
On the technology side, expect deeper integration with edge computing and federated learning, allowing real-time data processing and AI training at the source without compromising data privacy. This will unlock truly scalable, decentralized digital twin ecosystems – especially vital in rural or under-resourced regions.
Lastly, as patient digital twins become more portable, individuals could carry their own dynamic health models across providers, cities, and even countries – transforming continuity of care forever.
The future of digital twins in healthcare isn’t just smarter systems. It’s healthcare that learns, adapts, and heals ahead of time.
FAQs.
Q. What are digital twins in healthcare?
Ans.Digital twin technology in medicine are virtual replicas of real-world entities – such as a patient, organ, device, or entire hospital system – that use real-time data and simulation models to mirror, analyze, and predict behaviors. They integrate data from sources like EHRs, imaging, wearables, genomics, and IoT devices to support proactive, personalized care and smarter clinical decision-making.
Q. Why is digital twin technology gaining traction in healthcare?
Ans. As healthcare systems face increasing complexity – rising patient volumes, chronic disease burdens, and clinician burnout – digital twins offer a scalable way to improve decision-making, reduce trial-and-error in treatment, and streamline operations. Advances in AI, simulation modeling, and interoperability standards have made digital twin adoption more feasible and valuable than ever.
Q. What are the benefits of using digital twins in patient care?
Ans. Digital twins allow providers to simulate different treatment paths, predict outcomes, and intervene earlier – resulting in more personalized care with fewer complications. Benefits include better chronic disease management, precision treatment planning, faster post-op recovery, and fewer emergency readmissions. They also enable continuous monitoring through real-time data syncing with wearables or sensors.
Q. What challenges exist in adopting digital twins in hospitals?
Ans. Key challenges include fragmented data systems, high development costs, complex compliance requirements (like HIPAA and GDPR), and resistance to adoption by clinical staff. Building a reliable digital twin also requires deep cross-functional collaboration among clinicians, engineers, and data scientists – something not all healthcare systems are set up to support.
Q. Why choose CodingWorkX for healthcare AI or digital twin solutions?
Ans. CodingWorkX combines deep healthcare domain expertise with technical excellence in AI, simulation modeling, and system integration. We don’t just build digital twins – we help you identify the right use cases, align with regulatory standards, and design scalable, interoperable solutions that fit your workflow. From pilot to production, we’re a strategic partner every step of the way.
Q. How are digital twins being used in the medical field?
Ans. Digital twins are being used for surgical planning, chronic disease management, ICU demand forecasting, drug testing, equipment maintenance, and even mental health monitoring. They’re helping clinicians rehearse surgeries, test treatments virtually, detect early warning signs, and optimize hospital operations in real time.
Q. What are the key use cases of digital twin technology in healthcare?
Ans. Some of the most impactful use cases include:
- Simulating treatment options for cancer and other chronic conditions
- Personalizing post-op rehab plans
- Forecasting ICU bed demand and hospital resource allocation
- Preventive maintenance of critical equipment
- Enhancing clinical training through real-world simulations
- Monitoring behavioral health trends to preempt crises